Hälsa
Should dogs be vaccinated?
Recent debates about the safety of vaccines have many animal parents questioning whether their dogs should be vaccinated. The simple answer is absolutely!
Animals should receive core vaccines, which are absolutely necessary for all pets, and may require additional vaccines based on their lifestyle.
Little if any medicine is without risk, but the benefits of immunizing pets certainly overtake the few risks since many prevalent vaccinations in pets protect against life-threatening diseases like rabies.
Immunizations not only save animals but also help to prevent human illness.
The World Health Organization estimates that 59,000 people worldwide die of rabies every year, but only one or two of those fatalities take place in the United States, where laws demand that all animals be immunized.
Due to widespread vaccination, only a few pets contract rabies, and a small number of people are exposed.
Over 95% of rabies-related fatalities take place in Africa and Asia, where vaccination campaigns are unsuccessful.
Hälsa
Should dogs be vaccinated?
Recent debates about the safety of vaccines have many animal parents questioning whether their dogs should be vaccinated. The simple answer is absolutely! Animals should receive core vaccines, which are absolutely necessary for all pets, and may require additional vaccines based on their lifestyle.
Little if any medicine is without risk, but the benefits of immunizing pets certainly overtake the few risks since many prevalent vaccinations in pets protect against life-threatening diseases like rabies. Immunizations not only save animals but also help to prevent human illness.
The World Health Organization estimates that 59,000 people worldwide die of rabies every year, but only one or two of those fatalities take place in the United States, where laws demand that all animals be immunized. Due to widespread vaccination, only a few pets contract rabies, and a small number of people are exposed. Over 95% of rabies-related fatalities take place in Africa and Asia, where vaccination campaigns are unsuccessful.

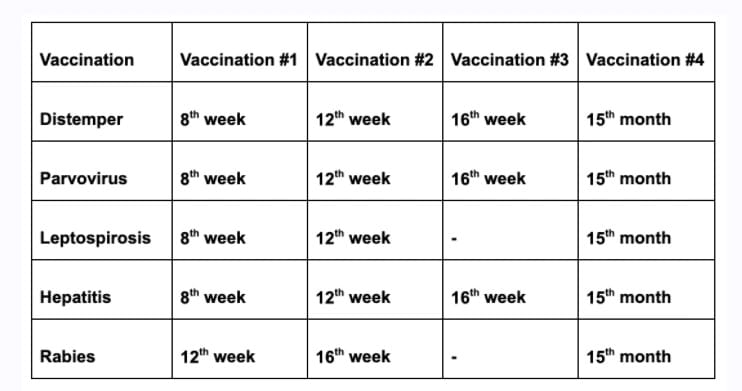
Swedish Kennel Club (Svenska Kennelklubben)- recommendation about dog vaccinations
The triple vaccine must be administered at 8 weeks, 12 weeks, and 12 months of age. Svenska Kennelklubben (SKK) recommends routine vaccinations every four years after that. It is critical that you clean up after your dog to avoid the spread of parvovirus.
For the most up-to-date vaccination information, contact the Swedish Board of Agriculture (www.sjv.se) or the country's embassy before traveling abroad.
Swedish Kennel Club (Svenska Kennelklubben)- recommendation about dog vaccinations
The triple vaccine must be administered at 8 weeks, 12 weeks, and 12 months of age. Svenska Kennelklubben (SKK) recommends routine vaccinations every four years after that. It is critical that you clean up after your dog to avoid the spread of parvovirus.
For the most up-to-date vaccination information, contact the Swedish Board of Agriculture (www.sjv.se) or the country's embassy before traveling abroad.

It is extremely crucial for dogs who reside in urban areas and interact with many other dogs to have adequate vaccination protection.
All puppies should receive a triple vaccine against parvovirus, canine distemper, and infectious canine hepatitis (HCC).
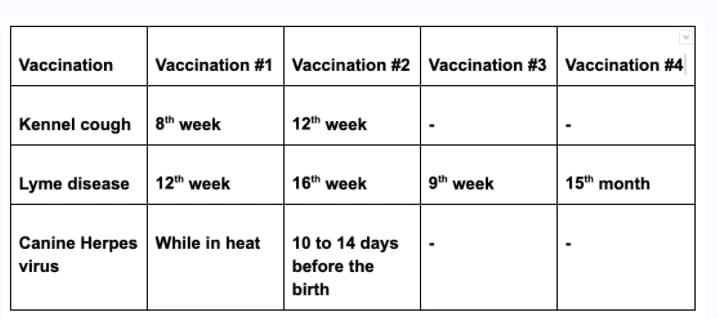
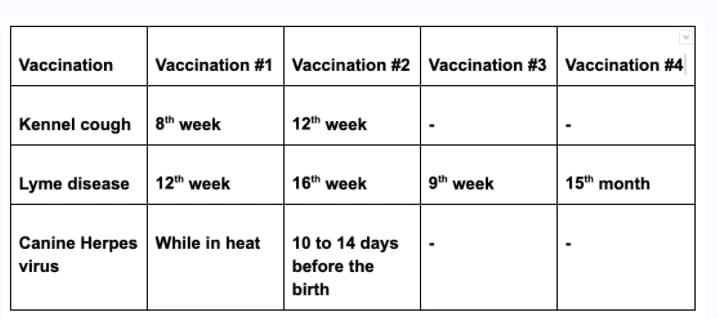
At the same time, puppies can be immunized against kennel cough.
As several dogs come in contact, the risk of kennel cough increases.
Always remain vigilant about your dog's health and take note of any changes. If he/she begins to cough, keep him/her isolated from other dogs to avoid infection spread. For more information, speak with your veterinarian.
Dogs getting fleas and lice is really common. If your dog seems to have caught some, you must bathe him/her with a special shampoo that is used to remove fleas and ticks.
You must also inform other dog owners that your dog had vermin. This will help to reduce the spread since the owners know that their pet might have fleas or ticks and bathe them.
Shampoo is available in pharmacies without a prescription. Preventive prescription preparations for both lice and ticks are also available.
It is extremely crucial for dogs who reside in urban areas and interact with many other dogs to have adequate vaccination protection. All puppies should receive a triple vaccine against parvovirus, canine distemper, and infectious canine hepatitis (HCC). At the same time, puppies can be immunized against kennel cough.
As several dogs come in contact, the risk of kennel cough increases. Always remain vigilant about your dog's health and take note of any changes. If he/she begins to cough, keep him/her isolated from other dogs to avoid infection spread. For more information, speak with your veterinarian.
Dogs getting fleas and lice is really common. If your dog seems to have caught some, you must bathe him/her with a special shampoo that is used to remove fleas and ticks. You must also inform other dog owners that your dog had vermin. This will help to reduce the spread since the owners know that their pet might have fleas or ticks and bathe them. Shampoo is available in pharmacies without a prescription. Preventive prescription preparations for both lice and ticks are also available.
Side effects of vaccinations for dogs
Side effects of vaccinations for dogs
Optional shots for dogs can cause concerns or health problems in some cases.
For instance, vaccination against the herpes virus in female dogs is a popular issue among dog owners, with some linking it to a high puppy mortality rate.
However, it is undeniable that mandatory vaccinations have significantly reduced the spread of diseases such as distemper, leptospirosis, parvovirus, and hepatitis.
These viruses and bacteria now kill very few to no dogs.
The most common vaccination complications are tissue swelling near the injection site, mild symptoms of disease such as fever, fatigue, and soreness, and allergic reactions to the vaccine that can vary from minor to life-threatening.
The risk of a worrisome reaction is low, but the risk of your pet developing a life-threatening illness is much higher if he is not immunized.
When you purchase a puppy, you accept responsibility for her/his life as well as the lives of other individuals and animals.
Several vaccinated dogs contribute to fewer dog deaths.
Even so, vaccinations for pets are not without complications. They feel the needle's entry point for a while afterward, just like people.
There will be a minor bump, but it will fade in about eight weeks. You should also expect your dog to appear more fatigued than usual for up to three days.
Make sure the dog gets sufficient rest and avoid overexerting it with long walks.
Major problems such as fever, appetite loss, swelling of the head, but also vomiting, shortness of breath, and weakness are less common, but not improbable. As a result, proper veterinary care is critical.
A trusted veterinarian can provide you with personalized advice about your pet.
Of course, your puppy must be completely healthy before being vaccinated.
If he/she develops an intolerance to a vaccine, a veterinarian can help.

Optional shots for dogs can cause concerns or health problems in some cases. For instance, vaccination against the herpes virus in female dogs is a popular issue among dog owners, with some linking it to a high puppy mortality rate.
However, it is undeniable that mandatory vaccinations have significantly reduced the spread of diseases such as distemper, leptospirosis, parvovirus, and hepatitis. These viruses and bacteria now kill very few to no dogs.
The most common vaccination complications are tissue swelling near the injection site, mild symptoms of disease such as fever, fatigue, and soreness, and allergic reactions to the vaccine that can vary from minor to life-threatening.
The risk of a worrisome reaction is low, but the risk of your pet developing a life-threatening illness is much higher if he is not immunized.
When you purchase a puppy, you accept responsibility for her/his life as well as the lives of other individuals and animals. Several vaccinated dogs contribute to fewer dog deaths.
Even so, vaccinations for pets are not without complications. They feel the needle's entry point for a while afterward, just like people. There will be a minor bump, but it will fade in about eight weeks. You should also expect your dog to appear more fatigued than usual for up to three days.
Make sure the dog gets sufficient rest and avoid overexerting it with long walks.
Major problems such as fever, appetite loss, swelling of the head, but also vomiting, shortness of breath, and weakness are less common, but not improbable. As a result, proper veterinary care is critical.
A trusted veterinarian can provide you with personalized advice about your pet.
Of course, your puppy must be completely healthy before being vaccinated.
If he/she develops an intolerance to a vaccine, a veterinarian can help.
What determines which vaccines should my pet receive?
Your veterinarian will assess your pet's exposure risk to determine whether he needs to be vaccinated against a specific disease.
Age: A particular vaccination protocol is required to assist puppies in developing disease resistance while the immunity passed down from their mothers wears off. Adult pets require booster vaccines after the early vaccine series to maintain immunity.
Geography: Some diseases have a higher risk of exposure in certain geographical regions; for example, Lyme disease is more common in largely forested areas, such as the Northeast.
Lifestyle: Dogs who often interact with other dogs, or have a greater exposure by going to a dog daycare (meeting a lot of dogs daily).

What determines which vaccines should my pet receive?
Your veterinarian will assess your pet's exposure risk to determine whether he needs to be vaccinated against a specific disease.
Age: A particular vaccination protocol is required to assist puppies in developing disease resistance while the immunity passed down from their mothers wears off. Adult pets require booster vaccines after the early vaccine series to maintain immunity.
Geography: Some diseases have a higher risk of exposure in certain geographical regions; for example, Lyme disease is more common in largely forested areas, such as the Northeast.
Lifestyle: Dogs who often interact with other dogs, or have a greater exposure by going to a dog daycare (meeting a lot of dogs daily).
Which core vaccines should a dog receive?
Based on the risk of exposure, the intensity of the disease, or transmissibility to humans, core vaccines are considered essential for all pets.
Canine distemper is a fatal disease that impacts the nervous and respiratory systems.
Hepatitis A and B: Hepatitis, caused by adenovirus type 1, can result in acute or chronic liver inflammation.
In unprotected puppies, parvovirus leads to significant vomiting, diarrhea, and dehydration, as well as life-threatening sepsis.
Rabies is a disease that causes gradual neurological problems and death. It is spread through bites from infected animals and can be transmitted to human beings.
Based on where your dog lives, her/his age, and her/his lifestyle, your veterinarian might well suggest the following supplemental vaccines for her/him:
Lyme disease: It is spread by the black-legged tick (Ixodes scapularis) and seems to be common in wooded areas.
Leptospirosis is caused by bacteria found in the urine of contaminated animals in the wild; pets and humans can become infected by drinking or having contact with the contaminated outdoor water and eventually develop liver and kidney failure.
Bordetella bronchiseptica is the pathogen responsible for kennel cough, a lung illness (respiratory) that is common in shelter dogs.
The parainfluenza virus causes respiratory infections in dogs; a single vaccine containing both the parainfluenza and the Bordetella bacteria can prevent kennel cough.
Canine influenza virus: This virus has recently been found to cause respiratory disease in dogs; immunization by vaccination is recommended for dogs who are exposed to other dogs from outside of the home.
Which core vaccines should a dog receive?
Based on the risk of exposure, the intensity of the disease, or transmissibility to humans, core vaccines are considered essential for all pets.
Canine distemper is a fatal disease that impacts the nervous and respiratory systems.
Hepatitis A and B: Hepatitis, caused by adenovirus type 1, can result in acute or chronic liver inflammation.
In unprotected puppies, parvovirus leads to significant vomiting, diarrhea, and dehydration, as well as life-threatening sepsis.
Rabies is a disease that causes gradual neurological problems and death. It is spread through bites from infected animals and can be transmitted to human beings.
Based on where your dog lives, her/his age, and her/his lifestyle, your veterinarian might well suggest the following supplemental vaccines for her/him:
Lyme disease: It is spread by the black-legged tick (Ixodes scapularis) and seems to be common in wooded areas.
Leptospirosis is caused by bacteria found in the urine of contaminated animals in the wild; pets and humans can become infected by drinking or having contact with the contaminated outdoor water and eventually develop liver and kidney failure.
Bordetella bronchiseptica is the pathogen responsible for kennel cough, a lung illness (respiratory) that is common in shelter dogs.
The parainfluenza virus causes respiratory infections in dogs; a single vaccine containing both the parainfluenza and the Bordetella bacteria can prevent kennel cough.
Canine influenza virus: This virus has recently been found to cause respiratory disease in dogs; immunization by vaccination is recommended for dogs who are exposed to other dogs from outside of the home.
Pets help with school anxiety
An American research of children aged 4 to 10 years old found that having a pet helps lessen anxiety in little children about going to school, being alone in the house, being extremely timid, and being scared for no apparent reason.
At the same time, a Croatian experiment (on war-traumatized youngsters) found no difference in self-esteem between children who had housepets and those who do not.
Vaccinations for an 8-week-old puppy
In the eighth week, your puppy receives its first vaccination from the veterinarian. This procedure is frequently handled by the breeder.
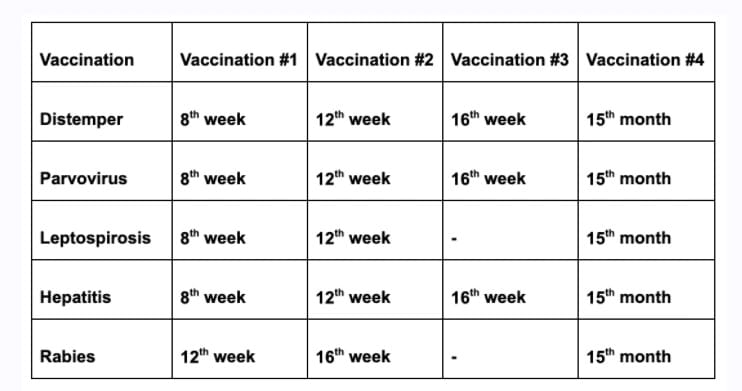
Vaccinations for an 8-week-old puppy
In the eighth week, your puppy receives its first vaccination from the veterinarian. This procedure is frequently handled by the breeder.
You must receive a vaccination certificate. This information will be included in your puppy's EU pet passport or vaccination card.
At this time, your dog should be safe against some of the diseases.
Pets help with school anxiety
An American research of children aged 4 to 10 years old found that having a pet helps lessen anxiety in little children about going to school, being alone in the house, being extremely timid, and being scared for no apparent reason.
At the same time, a Croatian experiment (on war-traumatized youngsters) found no difference in self-esteem between children who had housepets and those who do not.
You must receive a vaccination certificate. This information will be included in your puppy's EU pet passport or vaccination card. At this time, your dog should be safe against some of the diseases.
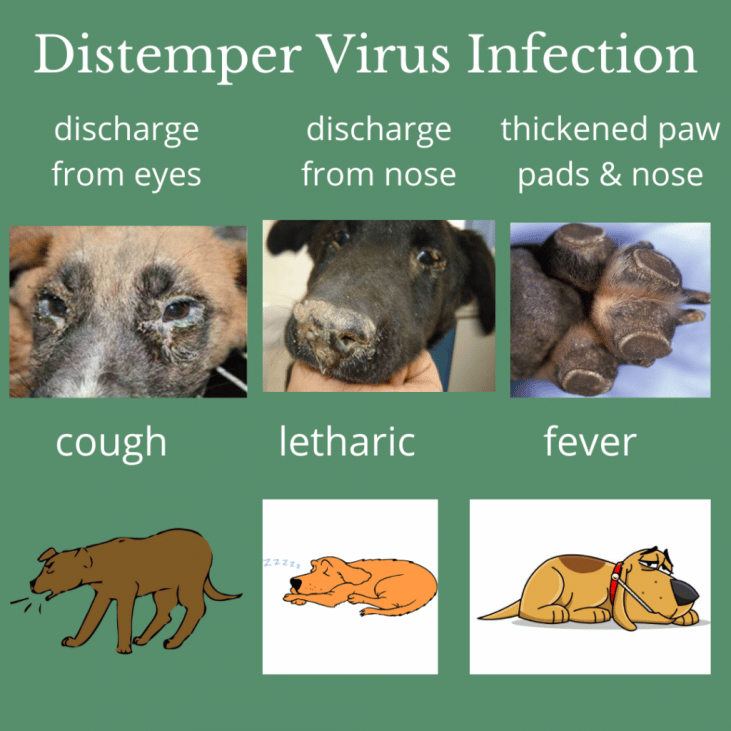
Canine distemper
Canine Distemper Virus-was among the most frequently fatal diseases in dogs until the late twentieth century. This viral infection affects both your dog's internal organs and nervous system. In addition to extreme brain and spinal cord damage, the dog's eyes, along with their dentition, are affected if the disease is caught before the initial tooth change. Since the introduction of mandatory distemper vaccination, these cases have become an exception.
How is it spread?
Puppies and dogs are most commonly infected by the virus from a highly contagious dog or wild animal through airborne exposure (sneezing or coughing).
The pathogen can also be spread through common food and water bowls, as well as equipment. Infected dogs can spread the pathogen for months, and mother dogs can transmit the virus to their puppies through the placenta.
Because canine distemper affects wildlife, interaction among animals in the wild and domestic dogs can help the virus spread.
What dogs are at risk?
All dogs are at risk of contracting the disease, but puppies under four months old and unvaccinated dogs are more vulnerable (there is an increased risk of them getting it).
Symptoms
Infected dogs will initially experience watery to pus-like discharge from their eyes.
Fever, nasal discharge, coughing, extreme fatigue, appetite loss, and vomiting follow. Infected dogs exhibit circling behavior, head shake, muscle spasms, seizures with jaw-nibbling movements and salivation, convulsions, and complete or partial paralysis as the virus infects the nervous system.
The virus may also cause footpads to thicken and harden, giving rise to the term "hard pad disease."
Canine distemper infection in wildlife is very similar to rabies.
Distemper is frequently fatal, and dogs who survive usually suffer permanent, irreversible nervous system damage.
How is it diagnosed and treated?
Canine distemper is diagnosed by veterinarians based on clinical signs and laboratory testing.
Canine distemper infection has no cure. Supportive care and measures to avoid secondary infections, control vomiting, diarrhea, and neurologic symptoms, and fight dehydration through fluid administration are typical treatments.
Canine distemper infected dogs must be kept separate from other animals to decrease the chance of further illness.
Preventive measures
The puppies are given a series of vaccines to build up their immune system.
Avoid gaps in the immunization and make sure your puppy is up to date with her/his vaccines.
Avoid contact with infected animals (including wild ones).
Use caution when socializing the puppy or unvaccinated dogs around dog parks, puppy classes, doggy daycare, and any other places you might visit with your dog and there are other dogs present.
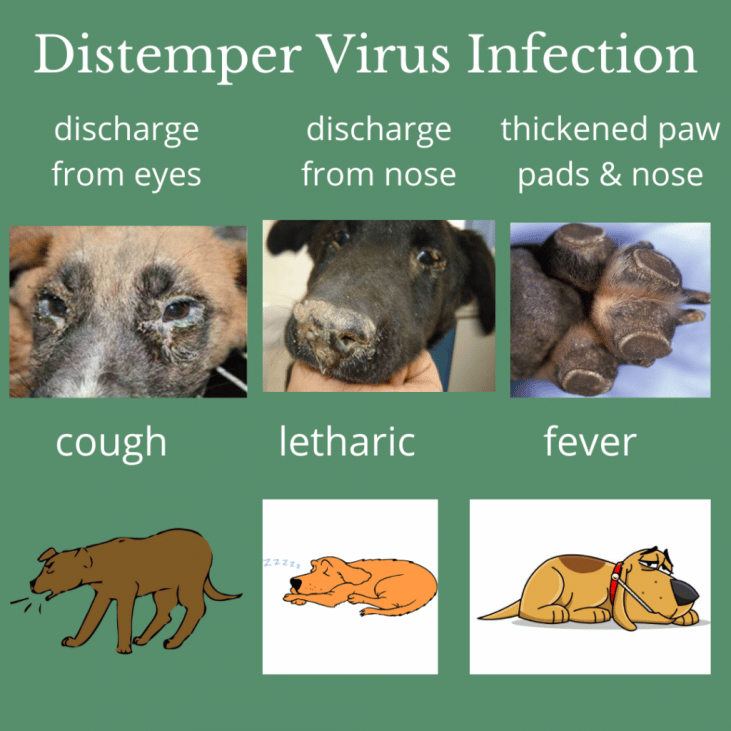
Canine distemper
Canine Distemper Virus-was among the most frequently fatal diseases in dogs until the late twentieth century. This viral infection affects both your dog's internal organs and nervous system. In addition to extreme brain and spinal cord damage, the dog's eyes, along with their dentition, are affected if the disease is caught before the initial tooth change. Since the introduction of mandatory distemper vaccination, these cases have become an exception.
How is it spread?
Puppies and dogs are most commonly infected by the virus from a highly contagious dog or wild animal through airborne exposure (sneezing or coughing). The pathogen can also be spread through common food and water bowls, as well as equipment. Infected dogs can spread the pathogen for months, and mother dogs can transmit the virus to their puppies through the placenta.
Because canine distemper affects wildlife, interaction among animals in the wild and domestic dogs can help the virus spread.
What dogs are at risk?
All dogs are at risk of contracting the disease, but puppies under four months old and unvaccinated dogs are more vulnerable (there is an increased risk of them getting it).
Symptoms
Infected dogs will initially experience watery to pus-like discharge from their eyes. Fever, nasal discharge, coughing, extreme fatigue, appetite loss, and vomiting follow. Infected dogs exhibit circling behavior, head shake, muscle spasms, seizures with jaw-nibbling movements and salivation, convulsions, and complete or partial paralysis as the virus infects the nervous system. The virus may also cause footpads to thicken and harden, giving rise to the term "hard pad disease."
Canine distemper infection in wildlife is very similar to rabies.
Distemper is frequently fatal, and dogs who survive usually suffer permanent, irreversible nervous system damage.
How is it diagnosed and treated?
Canine distemper is diagnosed by veterinarians based on clinical signs and laboratory testing. Canine distemper infection has no cure. Supportive care and measures to avoid secondary infections, control vomiting, diarrhea, and neurologic symptoms, and fight dehydration through fluid administration are typical treatments. Canine distemper infected dogs must be kept separate from other animals to decrease the chance of further illness.
Preventive measures
The puppies are given a series of vaccines to build up their immune system.
Avoid gaps in the immunization and make sure your puppy is up to date with her/his vaccines.
Avoid contact with infected animals (including wild ones).
Use caution when socializing the puppy or unvaccinated dogs around dog parks, puppy classes, doggy daycare, and any other places you might visit with your dog and there are other dogs present.
Additional information about the Canine Distemper Virus
Long-term conditions after the virus survival
A dog that recovers from distemper will always exhibit both non-life-threatening and life-threatening symptoms.
Hard pad disease, which causes the skin on the paw pads and the tip of the nose to harden, is the most frequent non-life-threatening symptom.
Enamel hypoplasia is another typical long-lasting symptom.
The enamel of teeth that are not fully developed or that have not yet erupted through the gums is especially vulnerable in puppies.
This happens as a result of the virus destroying the cells that produce tooth enamel. These teeth have the potential to decay quickly.
Typically, nervous system degenerative symptoms are among the most serious ones.
Distemper-infected dogs frequently experience a gradual decline in their mental and physical ability.
The dog may eventually experience increasingly severe seizures, paralysis, vision loss, and incoordination.
Due to the extreme hardship these dogs endure, they are typically euthanized mercifully.
Mechanism and diagnosis
Nearly all bodily systems are impacted by the canine distemper virus.
Puppies between three and six months old are especially vulnerable.
Six to 22 days after exposure, CDV spreads by aerosol droplets and through contact with bodily fluids containing the virus, such as nasal and ocular secretions, feces, and urine.
Food and drink infected with these fluids can potentially spread it. There are 14 to 18 days between an infection and a sickness, while a fever might start 3 to 6 days after infection.
The preceding symptoms, particularly fever, respiratory and neurological symptoms, thicker footpads, and other indicators that appear in uninfected dogs, strongly suggest CDV.
However, a number of febrile illnesses mimic many of the symptoms of the illness, and it has only lately become able to tell canine hepatitis, herpes virus, parainfluenza, and leptospirosis apart.

Long-term conditions after the virus survival
A dog that recovers from distemper will always exhibit both non-life-threatening and life-threatening symptoms. Hard pad disease, which causes the skin on the paw pads and the tip of the nose to harden, is the most frequent non-life-threatening symptom. Enamel hypoplasia is another typical long-lasting symptom.
The enamel of teeth that are not fully developed or that have not yet erupted through the gums is especially vulnerable in puppies. This happens as a result of the virus destroying the cells that produce tooth enamel. These teeth have the potential to decay quickly.
Typically, nervous system degenerative symptoms are among the most serious ones. Distemper-infected dogs frequently experience a gradual decline in their mental and physical ability.
The dog may eventually experience increasingly severe seizures, paralysis, vision loss, and incoordination. Due to the extreme hardship these dogs endure, they are typically euthanized mercifully.
Mechanism and diagnosis
Nearly all bodily systems are impacted by the canine distemper virus.
Puppies between three and six months old are especially vulnerable. Six to 22 days after exposure, CDV spreads by aerosol droplets and through contact with bodily fluids containing the virus, such as nasal and ocular secretions, feces, and urine.
Food and drink infected with these fluids can potentially spread it. There are 14 to 18 days between an infection and a sickness, while a fever might start 3 to 6 days after infection.
The preceding symptoms, particularly fever, respiratory and neurological symptoms, thicker footpads, and other indicators that appear in uninfected dogs, strongly suggest CDV.
However, a number of febrile illnesses mimic many of the symptoms of the illness, and it has only lately become able to tell canine hepatitis, herpes virus, parainfluenza, and leptospirosis apart.
Additional information about the Canine Distemper Virus
Parvovirus
This nefarious virus, sometimes known as the dog plague, is especially harmful to puppies.
Excretions by the roadway are a common way for it to spread. Your dog will have bloody diarrhea. In the worst scenarios, fluid loss can result in the dog's death.
This disease was just identified about 40 years ago, and as of today, the only ways to prevent it are vaccination and prompt veterinary care.
The majority of parvovirus deaths happen 48 to 72 hours after the appearance of clinical symptoms. The moment your dog or puppy exhibits any of these symptoms, you should call your veterinarian.
How is it spread?
Direct contact between dogs as well as contact with contaminated environments, humans, or excrement (stool) are the two main ways in which the virus, which affects dogs' gastrointestinal tracts, spreads. Infected dog handlers' hands, clothing, water, food bowls, collars, and kennel floors can all get contaminated with the virus.
It can survive for a long time in the environment and is able to withstand heat, cold, humidity, and dryness.
Any quantity of a virus-carrying dog's feces can spread the disease to other dogs that come into contact with them.
The infection can easily spread from one location to another on dog hair or feet, as well as through contaminated cages, shoes, and other items.
What dogs are at risk?
All dogs are susceptible to the extremely contagious canine parvovirus, however, pups under four months old and unvaccinated canines are particularly at risk.
Symptoms
Fatigue, a lack of appetite, abdominal pain and bloating, fever or low body temperature (hypothermia), vomiting, and severe, frequently bloody diarrhea are some of the symptoms of parvovirus.
Intestinal and immunological damage can result in septic shock, and continuous vomiting and diarrhea will quickly dehydrate the dog's body.
How is it diagnosed and treated
On the basis of the dog's medical history, physical exam, and laboratory tests, parvovirus infection is frequently suspected.
The diagnosis can be verified by fecal tests.
There isn't a specific medication that can eradicate the disease in infected dogs, so the goal of treatment is to support the body systems of the dog until its immune system can eradicate the viral infection.
The primary goals of treatment, which should begin right once, are to counteract dehydration by replenishing electrolytes, protein, and fluid losses, managing vomiting and diarrhea, and avoiding subsequent infections.
Dogs who are ill must stay warm and be given expert nursing care.
Even with rigorous treatment, a dog with parvo may not survive and treatment for it can be quite expensive.
Successful outcomes heavily depend on early detection and vigorous treatment.
With the right care, survival rates can get close to 90%.
Since parvovirus is extremely contagious, it is essential to isolate affected dogs in order to prevent infection from spreading.
Controlling the spread of parvovirus requires thorough disinfection and cleaning of infected kennels and other locations where diseased canines are (or have been) housed.
Because the virus is difficult to eradicate, speak with your veterinarian for advice on the best cleaning and disinfecting solutions.
Preventive measures
Both vaccinations and basic hygiene are essential for prevention.
Young puppies are particularly vulnerable to infection because their mothers' milk's natural immunity may wear out before the puppies' own immune function is developed enough to combat infection.
Puppy illness is possible if canine parvovirus exposure occurs at this time of reduced immunity.
Another issue is that a mother's milk immunity may prevent a child from responding to a vaccination effectively.
This means that even puppies who have received vaccinations may occasionally contract the parvovirus and become ill.
Depending on how many doses they have previously gotten, dogs must receive a dose of the canine parvovirus vaccination between the ages of 14 and 16 weeks old in order to develop an appropriate defense.
Owners of adult dogs should ensure that their canines are current on their parvovirus vaccinations in order to protect them.
The number of antibodies a dog has against the canine parvovirus can be measured using titers, however, exposure to the virus may not necessarily result in protection.
Inquire with the vet about the best preventative strategy for your dog.
When taking their pet to areas where young puppies congregate, pet owners should use caution until their pet has gotten the full set of immunizations ( pet shops, parks, puppy classes, obedience classes, doggy daycare, kennels, and grooming establishments).
By requiring immunizations, health checks, excellent hygiene, and isolation of sick puppies and dogs, respectable facilities and training programs lower the chance of exposure.
Always avoid coming into contact with known diseased canines and their properties.
Finally, avoid letting your dog—adult or puppy—touch other dogs' excrement while out for a walk or outside play.
It is always advisable to dispose of waste materials promptly and properly in order to prevent the transmission of diseases that can affect both humans and animals, such as the canine parvovirus infection.
It is not advisable to bring sick dogs or other dogs who have been exposed to sick dogs to kennels, dog parks, or other places where they may interact with other dogs.
When handling other dogs, those who have been in contact with sick or exposed dogs should refrain, or at the very least wash their hands and change their clothes.
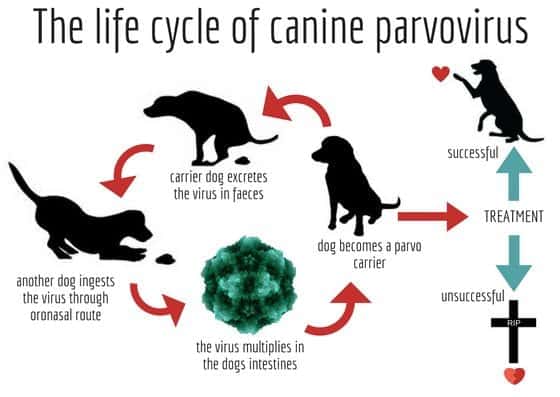
Parvovirus
This nefarious virus, sometimes known as the dog plague, is especially harmful to puppies. Excretions by the roadway are a common way for it to spread. Your dog will have bloody diarrhea. In the worst scenarios, fluid loss can result in the dog's death. This disease was just identified about 40 years ago, and as of today, the only ways to prevent it are vaccination and prompt veterinary care.
The majority of parvovirus deaths happen 48 to 72 hours after the appearance of clinical symptoms. The moment your dog or puppy exhibits any of these symptoms, you should call your veterinarian.
How is it spread?
Direct contact between dogs as well as contact with contaminated environments, humans, or excrement (stool) are the two main ways in which the virus, which affects dogs' gastrointestinal tracts, spreads. Infected dog handlers' hands, clothing, water, food bowls, collars, and kennel floors can all get contaminated with the virus. It can survive for a long time in the environment and is able to withstand heat, cold, humidity, and dryness.
Any quantity of a virus-carrying dog's feces can spread the disease to other dogs that come into contact with them. The infection can easily spread from one location to another on dog hair or feet, as well as through contaminated cages, shoes, and other items.
What dogs are at risk?
All dogs are susceptible to the extremely contagious canine parvovirus, however, pups under four months old and unvaccinated canines are particularly at risk.
Symptoms
Fatigue, a lack of appetite, abdominal pain and bloating, fever or low body temperature (hypothermia), vomiting, and severe, frequently bloody diarrhea are some of the symptoms of parvovirus. Intestinal and immunological damage can result in septic shock, and continuous vomiting and diarrhea will quickly dehydrate the dog's body.
How is it diagnosed and treated
On the basis of the dog's medical history, physical exam, and laboratory tests, parvovirus infection is frequently suspected. The diagnosis can be verified by fecal tests.
There isn't a specific medication that can eradicate the disease in infected dogs, so the goal of treatment is to support the body systems of the dog until its immune system can eradicate the viral infection. The primary goals of treatment, which should begin right once, are to counteract dehydration by replenishing electrolytes, protein, and fluid losses, managing vomiting and diarrhea, and avoiding subsequent infections.
Dogs who are ill must stay warm and be given expert nursing care. Even with rigorous treatment, a dog with parvo may not survive and treatment for it can be quite expensive. Successful outcomes heavily depend on early detection and vigorous treatment.
With the right care, survival rates can get close to 90%.
Since parvovirus is extremely contagious, it is essential to isolate affected dogs in order to prevent infection from spreading. Controlling the spread of parvovirus requires thorough disinfection and cleaning of infected kennels and other locations where diseased canines are (or have been) housed. Because the virus is difficult to eradicate, speak with your veterinarian for advice on the best cleaning and disinfecting solutions.
Preventive measures
Both vaccinations and basic hygiene are essential for prevention.
Young puppies are particularly vulnerable to infection because their mothers' milk's natural immunity may wear out before the puppies' own immune function is developed enough to combat infection. Puppy illness is possible if canine parvovirus exposure occurs at this time of reduced immunity. Another issue is that a mother's milk immunity may prevent a child from responding to a vaccination effectively.
This means that even puppies who have received vaccinations may occasionally contract the parvovirus and become ill. Depending on how many doses they have previously gotten, dogs must receive a dose of the canine parvovirus vaccination between the ages of 14 and 16 weeks old in order to develop an appropriate defense.
Owners of adult dogs should ensure that their canines are current on their parvovirus vaccinations in order to protect them. The number of antibodies a dog has against the canine parvovirus can be measured using titers, however, exposure to the virus may not necessarily result in protection. Inquire with the vet about the best preventative strategy for your dog.
When taking their pet to areas where young puppies congregate, pet owners should use caution until their pet has gotten the full set of immunizations ( pet shops, parks, puppy classes, obedience classes, doggy daycare, kennels, and grooming establishments).
By requiring immunizations, health checks, excellent hygiene, and isolation of sick puppies and dogs, respectable facilities and training programs lower the chance of exposure. Always avoid coming into contact with known diseased canines and their properties.
Finally, avoid letting your dog—adult or puppy—touch other dogs' excrement while out for a walk or outside play. It is always advisable to dispose of waste materials promptly and properly in order to prevent the transmission of diseases that can affect both humans and animals, such as the canine parvovirus infection.
It is not advisable to bring sick dogs or other dogs who have been exposed to sick dogs to kennels, dog parks, or other places where they may interact with other dogs. When handling other dogs, those who have been in contact with sick or exposed dogs should refrain, or at the very least wash their hands and change their clothes.
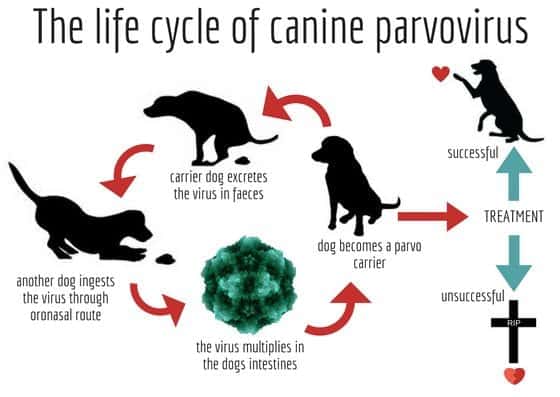
Additional information about Parvovirus
Vaccines can offer protection against this virus, but untreated cases can result in a 91% mortality rate. Animals frequently need to be hospitalized for treatment.
Among the mammals that are commonly infected with canine parvovirus include foxes, wolves, cats, and skunks. Cats are also prone to panleukopenia, a particular parvovirus strain.
Intestinal and cardiac form
Via oral contamination with CPV2 in feces, infected soil, or fomites that contain the virus, dogs can get infected.
After being consumed, the virus multiplies in the lymphoid tissue of the throat before entering the bloodstream.
From there, the virus targets cells that divide quickly, particularly those found in the bone marrow, lymph nodes, and intestinal crypts.
The lymph nodes' lymphocyte counts are reduced, and the intestinal crypts are necrotic and destroyed.
This less frequent variety affects puppies from the time of infection in the womb or soon after birth until they are about 8 weeks old.
When the virus targets the heart muscle, the puppy frequently passes away unexpectedly or just briefly has breathing problems brought on by pulmonary edema.
There are several microscopic sites of cardiac muscle necrosis that are connected to mononuclear cellular infiltration.
Even less commonly, the illness may induce lesions, viral multiplication, and attacks in regions other than the digestive tissues and heart, such as the brain, liver, lungs, kidneys, and adrenal cortex.
It may also result in a widespread illness in newborns. The vascular lining is also badly impacted, which causes the ulcers in this area to bleed.
The pathogen is quite resilient and can be found to last up to a year in soil, dung, and other organic compounds.
It can endure temperatures both very low and very high.
Bleach is the only household cleaner that can eradicate the infection. To sanitize and kill parvovirus, a 1:10 solution of diluted bleach is required.
Additional information about Parvovirus
Vaccines can offer protection against this virus, but untreated cases can result in a 91% mortality rate. Animals frequently need to be hospitalized for treatment. Among the mammals that are commonly infected with canine parvovirus include foxes, wolves, cats, and skunks. Cats are also prone to panleukopenia, a particular parvovirus strain.
Intestinal and cardiac form
Via oral contamination with CPV2 in feces, infected soil, or fomites that contain the virus, dogs can get infected. After being consumed, the virus multiplies in the lymphoid tissue of the throat before entering the bloodstream. From there, the virus targets cells that divide quickly, particularly those found in the bone marrow, lymph nodes, and intestinal crypts.
The lymph nodes' lymphocyte counts are reduced, and the intestinal crypts are necrotic and destroyed.
This less frequent variety affects puppies from the time of infection in the womb or soon after birth until they are about 8 weeks old.
When the virus targets the heart muscle, the puppy frequently passes away unexpectedly or just briefly has breathing problems brought on by pulmonary edema. There are several microscopic sites of cardiac muscle necrosis that are connected to mononuclear cellular infiltration.
Even less commonly, the illness may induce lesions, viral multiplication, and attacks in regions other than the digestive tissues and heart, such as the brain, liver, lungs, kidneys, and adrenal cortex. It may also result in a widespread illness in newborns.
The vascular lining is also badly impacted, which causes the ulcers in this area to bleed. The pathogen is quite resilient and can be found to last up to a year in soil, dung, and other organic compounds. It can endure temperatures both very low and very high. Bleach is the only household cleaner that can eradicate the infection. To sanitize and kill parvovirus, a 1:10 solution of diluted bleach is required.

Leptospirosis

The worst-case situation for this illness is severe liver and kidney damage. It is spread by bacteria.
Dogs typically contract it from contact with rodent excrements, such as that of rats and hedgehogs, or by drinking stagnant water. Through the mucous membrane, the pathogen enters the blood.
Leptospirosis may not always manifest itself physically, but your dog will still carry the infection and be able to spread it to other dogs and even humans.
How is it spread?
Leptospirosis is a condition carried on by Leptospira bacterial infection. These bacteria are present in water and soil all around the planet.
Numerous Leptospira pathogens varieties can be harmful.
Leptospirosis can be transmitted from animals to humans since it is a zoonotic illness. Individuals who are infected may experience flu-like symptoms as well as liver or renal problems.
The vast majority of human leptospirosis cases in the US are caused by water-related leisure activities.
It is considerably less likely, but it is conceivable, to contract an infection after coming into contact with a diseased pet.
Although it can happen worldwide, leptospirosis is more prevalent in regions with hot climates and substantial yearly rainfall.-link
Who is at risk?
Humans and animals
Risk factors
Most often, dogs are impacted. Even though there is a lack of data regarding the illness in cats, leptospirosis in these animals is rare and seems to be moderate.
Wandering on farmlands (because of encountering potentially highly contagious wildlife, farm animals, or water sources), exposure to a wild animal or farm animal species, even if only in the backyard, contact with rodents, or contact with other dogs are all common risks factors for leptospirosis in dogs living in the United States.
Dogs can contract leptospirosis and become infected if their mucosal tissue (or skin with any lesion, such as a tear or cut) comes into contact with contaminated soil, water, food, or bedding from an infected animal; if they bite an infected animal; if they eat contaminated tissues or carcasses; or, very rarely, if they are bred with an infected animal.
It can also be transferred from the mother dog to the offspring through the placenta.
Symptoms
There are various canine leptospirosis symptoms.
Some infected dogs exhibit no symptoms at all, while others experience a mild disease that passes quickly and recovers on its own, while yet others experience a severe illness that results in death.
Leptospirosis symptoms can include fever, shivering, tenderness in the muscles, apprehension about moving around, extreme thirst, modifications in the frequency or quantity of urination, dehydration, vomiting, diarrhea, lack of appetite, lethargic behavior, jaundice (yellowing of the skin and mucous membranes), or uncomfortable eye inflammation.
The condition may result in either liver failure or renal failure. On rare occasions, dogs may acquire serious lung disease and experience breathing problems.
Leptospirosis can result in bleeding problems that can include nosebleeds, blood-tinged saliva, urine, feces, or vomit, and tiny red spots (which may be visible on the gums and other mucous membranes or on light-colored skin).
Affected dogs may also experience fluid buildup in their chests or abdomens or develop swollen legs.
How is it diagnosed?
Based on the dog's symptoms and exposure history, leptospirosis may be suspected, however many of these symptoms are also present in other diseases.
Your veterinarian may advise a number of further tests in addition to a physical examination, including blood tests, urine tests, radiographs (x-rays), and ultrasound examinations.
How is it treated?
Typically, supportive care and medicines are used to treat leptospirosis.
The likelihood of recovery is good with prompt and intensive treatment, but there is a danger of long-lasting kidney or liver damage.
Preventive measures
Leptospirosis can be prevented with currently available vaccines, which offer dogs protection for at least 12 months. For dogs who are at risk, annual vaccination is advised.
Your dog's risk of infection can be decreased by limiting its exposure to potential carriers of the Leptospira bacteria.
If your dog is already infected, wear gloves every time you need to clean a urine accident (quickly sanitize and disinfect the area), wash your hands after handling your pet, administer antibiotics (prescribed by the veterinarian) and encourage the dog to urinate away from standing water or from places that are frequently visited by other animals and people.
Leptospirosis
The worst-case situation for this illness is severe liver and kidney damage. It is spread by bacteria. Dogs typically contract it from contact with rodent excrements, such as that of rats and hedgehogs, or by drinking stagnant water. Through the mucous membrane, the pathogen enters the blood. Leptospirosis may not always manifest itself physically, but your dog will still carry the infection and be able to spread it to other dogs and even humans.
How is it spread?
Leptospirosis is a condition carried on by Leptospira bacterial infection. These bacteria are present in water and soil all around the planet. Numerous Leptospira pathogens varieties can be harmful. Leptospirosis can be transmitted from animals to humans since it is a zoonotic illness. Individuals who are infected may experience flu-like symptoms as well as liver or renal problems. The vast majority of human leptospirosis cases in the US are caused by water-related leisure activities. It is considerably less likely, but it is conceivable, to contract an infection after coming into contact with a diseased pet.
Although it can happen worldwide, leptospirosis is more prevalent in regions with hot climates and substantial yearly rainfall.-link
Who is at risk?
Humans and animals
Risk factors
Most often, dogs are impacted. Even though there is a lack of data regarding the illness in cats, leptospirosis in these animals is rare and seems to be moderate. Wandering on farmlands (because of encountering potentially highly contagious wildlife, farm animals, or water sources), exposure to a wild animal or farm animal species, even if only in the backyard, contact with rodents, or contact with other dogs are all common risks factors for leptospirosis in dogs living in the United States.
Dogs can contract leptospirosis and become infected if their mucosal tissue (or skin with any lesion, such as a tear or cut) comes into contact with contaminated soil, water, food, or bedding from an infected animal; if they bite an infected animal; if they eat contaminated tissues or carcasses; or, very rarely, if they are bred with an infected animal. It can also be transferred from the mother dog to the offspring through the placenta.
Symptoms
There are various canine leptospirosis symptoms. Some infected dogs exhibit no symptoms at all, while others experience a mild disease that passes quickly and recovers on its own, while yet others experience a severe illness that results in death.
Leptospirosis symptoms can include fever, shivering, tenderness in the muscles, apprehension about moving around, extreme thirst, modifications in the frequency or quantity of urination, dehydration, vomiting, diarrhea, lack of appetite, lethargic behavior, jaundice (yellowing of the skin and mucous membranes), or uncomfortable eye inflammation. The condition may result in either liver failure or renal failure. On rare occasions, dogs may acquire serious lung disease and experience breathing problems.
Leptospirosis can result in bleeding problems that can include nosebleeds, blood-tinged saliva, urine, feces, or vomit, and tiny red spots (which may be visible on the gums and other mucous membranes or on light-colored skin). Affected dogs may also experience fluid buildup in their chests or abdomens or develop swollen legs.
How is it diagnosed?
Based on the dog's symptoms and exposure history, leptospirosis may be suspected, however many of these symptoms are also present in other diseases. Your veterinarian may advise a number of further tests in addition to a physical examination, including blood tests, urine tests, radiographs (x-rays), and ultrasound examinations.
How is it treated?
Typically, supportive care and medicines are used to treat leptospirosis. The likelihood of recovery is good with prompt and intensive treatment, but there is a danger of long-lasting kidney or liver damage.
Preventive measures
Leptospirosis can be prevented with currently available vaccines, which offer dogs protection for at least 12 months. For dogs who are at risk, annual vaccination is advised. Your dog's risk of infection can be decreased by limiting its exposure to potential carriers of the Leptospira bacteria.
If your dog is already infected, wear gloves every time you need to clean a urine accident (quickly sanitize and disinfect the area), wash your hands after handling your pet, administer antibiotics (prescribed by the veterinarian) and encourage the dog to urinate away from standing water or from places that are frequently visited by other animals and people.

Hepatitis
For dogs, hepatitis is still frequently fatal. They are exposed to the virus by sick animals, which then infect the dog's liver.
Although the long-term chronic progression of the disease is often common, it can sometimes result in very abrupt, severe disease progression.
The liver's capacity then gradually deteriorates.
Additionally, people are not immune to this viral illness. It will show signs of pain in the upper abdomen, reddish mucus membranes, hazy eyes, increased bleeding, and increased bleeding in your dog.
Types of hepatitis
Canine infectious hepatitis and canine chronic hepatitis are the two kinds of hepatitis that are frequently observed in dogs.
A chronic infection is one that has been causing harm for a while (at least a few weeks), whereas acute hepatitis can show symptoms within a short period of time, such as a few days.
Infectious Hepatitis in Dogs
Canine adenovirus 1 causes the acute contagious illness infectious canine hepatitis, which affects dogs. The infected pet's liver, lungs, kidneys, spleen, blood vessel lining, and occasionally other organs are the targets of the virus.
Infectious canine hepatitis symptoms can range greatly, from mild fever to death.
Chronic Hepatitis in Dogs
A disorder known as infectious canine hepatitis is known as canine chronic hepatitis.
Skye Terriers, Springer Spaniels, Beagles, West Highland White Terriers, Cocker Spaniels, Maltese, Labrador Retrievers, Doberman Pinschers, Bedlington Terriers, Standard Poodles, and Chihuahuas are among the dog breeds that are susceptible to the condition.
How is it spread?
Dogs become infected by ingesting bodily fluids from other dogs (urine, feces, nasal discharge, or saliva).
After they recover the pathogen will still be present in their urine for at least 6 months. It is also possible for dogs who develop chronic hepatitis that they accumulated copper in their liver cells.
Symptoms
Eye and nasal discharge that is watery
Congestion
Mild fever
Blood clotting difficulty
Blindness
Decreased appetite
Thirst
Increased tonsils
Ears, gums, and skin that seem yellow and jaundiced
Eye irritation
Profound depression
Abdominal pain (occasional)
Vomiting (occasional)
Reddened or bruised mouth and nose
Unexpected bleeding
Extreme cases:
Skin with red spots
Reddened or bruised lips and nose
Swelling (neck, head, lymph nodes)
Seizures
Death
How is it diagnosed?
Infectious canine hepatitis is typically the cause of the condition's quick onset and bleeding, although laboratory testing (such as blood tests, immuno-fluorescence scans, and antibody tests) are required to make the diagnosis.
If your dog is very sick, blood transfusions can be necessary.
Routine blood tests may occasionally detect chronic hepatitis, allowing for a diagnosis before symptoms appear.
When your dog shows signs of liver disease, it's frequently already extremely late in the process.
A liver biopsy, which identifies the type and extent of liver illness your dog has, can provide a conclusive diagnosis.
How is it treated?
Depending on the findings of the biopsy, your veterinarian might advise using a broad-spectrum antibiotic, an anti-inflammatory drug, or an immunosuppressive drug to treat the illness.
The corneal clouding in the eye might occasionally be accompanied by an agonizing spasm.
To relieve your pup's discomfort, ask your veterinarian about an eye ointment. Protecting your dog's eye from intense light is crucial if they have corneal clouding.
Hospitalization and intravenous fluid therapy are both possible treatment options. For monitoring purposes, your dog will need regular blood work.
Long-term conditions after survival
Immune-complex reactions can cause renal damage over the long run and corneal clouding after the disease has been treated.
While chronic hepatitis cannot be healed but can be managed so that your dog lives a long, healthy life with few clinical indications, unlike acute hepatitis, which can sometimes be treated.
Preventive measures
The most popular and significant form of protection for contagious canine hepatitis is a vaccine that is required.
This immunization is often given to your dog at the same time as their canine distemper shots.
Puppies usually receive their first dose of the hepatitis vaccination between the ages of 7 and 9 weeks, followed by a second dose between the ages of 11 and 13 weeks, after which they become protected.
Your dog will require booster shots for the rest of its life to remain protected against this dangerous ailment – another one at 15 months, then every year to keep the infection away.

Hepatitis
For dogs, hepatitis is still frequently fatal. They are exposed to the virus by sick animals, which then infect the dog's liver. Although the long-term chronic progression of the disease is often common, it can sometimes result in very abrupt, severe disease progression. The liver's capacity then gradually deteriorates. Additionally, people are not immune to this viral illness. It will show signs of pain in the upper abdomen, reddish mucus membranes, hazy eyes, increased bleeding, and increased bleeding in your dog.
Types of hepatitis
Canine infectious hepatitis and canine chronic hepatitis are the two kinds of hepatitis that are frequently observed in dogs. A chronic infection is one that has been causing harm for a while (at least a few weeks), whereas acute hepatitis can show symptoms within a short period of time, such as a few days.
Infectious Hepatitis in Dogs
Canine adenovirus 1 causes the acute contagious illness infectious canine hepatitis, which affects dogs. The infected pet's liver, lungs, kidneys, spleen, blood vessel lining, and occasionally other organs are the targets of the virus. Infectious canine hepatitis symptoms can range greatly, from mild fever to death.
Chronic Hepatitis in Dogs
A disorder known as infectious canine hepatitis is known as canine chronic hepatitis. Skye Terriers, Springer Spaniels, Beagles, West Highland White Terriers, Cocker Spaniels, Maltese, Labrador Retrievers, Doberman Pinschers, Bedlington Terriers, Standard Poodles, and Chihuahuas are among the dog breeds that are susceptible to the condition.
How is it spread?
Dogs become infected by ingesting bodily fluids from other dogs (urine, feces, nasal discharge, or saliva). After they recover the pathogen will still be present in their urine for at least 6 months. It is also possible for dogs who develop chronic hepatitis that they accumulated copper in their liver cells.
Symptoms
Eye and nasal discharge that is watery
Congestion
Mild fever
Blood clotting difficulty
Blindness
Decreased appetite
Thirst
Increased tonsils
Ears, gums, and skin that seem yellow and jaundiced
Eye irritation
Profound depression
Abdominal pain (occasional)
Vomiting (occasional)
Reddened or bruised mouth and nose
Unexpected bleeding
Extreme cases:
Skin with red spots
Reddened or bruised lips and nose
Swelling (neck, head, lymph nodes)
Seizures
Death
How is it diagnosed?
Infectious canine hepatitis is typically the cause of the condition's quick onset and bleeding, although laboratory testing (such as blood tests, immuno-fluorescence scans, and antibody tests) are required to make the diagnosis. If your dog is very sick, blood transfusions can be necessary.
Routine blood tests may occasionally detect chronic hepatitis, allowing for a diagnosis before symptoms appear. When your dog shows signs of liver disease, it's frequently already extremely late in the process. A liver biopsy, which identifies the type and extent of liver illness your dog has, can provide a conclusive diagnosis.
How is it treated?
Depending on the findings of the biopsy, your veterinarian might advise using a broad-spectrum antibiotic, an anti-inflammatory drug, or an immunosuppressive drug to treat the illness.
The corneal clouding in the eye might occasionally be accompanied by an agonizing spasm. To relieve your pup's discomfort, ask your veterinarian about an eye ointment. Protecting your dog's eye from intense light is crucial if they have corneal clouding.
Hospitalization and intravenous fluid therapy are both possible treatment options. For monitoring purposes, your dog will need regular blood work.
Long-term conditions after survival
Immune-complex reactions can cause renal damage over the long run and corneal clouding after the disease has been treated. While chronic hepatitis cannot be healed but can be managed so that your dog lives a long, healthy life with few clinical indications, unlike acute hepatitis, which can sometimes be treated.
Preventive measures
The most popular and significant form of protection for contagious canine hepatitis is a vaccine that is required. This immunization is often given to your dog at the same time as their canine distemper shots.
Puppies usually receive their first dose of the hepatitis vaccination between the ages of 7 and 9 weeks, followed by a second dose between the ages of 11 and 13 weeks, after which they become protected.
Your dog will require booster shots for the rest of its life to remain protected against this dangerous ailment – another one at 15 months, then every year to keep the infection away.

Rabies
It is an incurable virus that attacks the brain and spinal cord. All mammals are susceptible to rabies. Even if it is preventable by vaccine and even treatable very early on, once the symptoms appear there is only an inevitable end.
How does it spread?
Since rabies is usually spread by a bite wound from an infected animal since it is produced in saliva.
The virus invades the bloodstream when the skin is punctured by a bite. It can also spread through an open sore that is licked by an infected animal and exposed to its saliva.
Although it can spread from pet to pet, interaction with wild animals like bats, raccoons, and foxes is the main cause of rabies in dogs.
About 400 to 500 cases of rabies in household pets such cats, dogs, and ferrets are reported each year. Due to vaccination, rabies is entirely preventable in dogs in the U.s, hence it is not particularly prevalent.
Symptoms
Watch closely your dog's actions and call your veterinarian right away if you have any suspicions of rabies or if your dog has been injured by another animal and you feel worried about it.
Your dog might exhibit hostility while also quickly becoming aggressive and restless.
Animals that are rabid may also exhibit unusually warm behavior (affectionate). Similar to this, your dog could appear relaxed and uninterested if they are typically joyful and excited.
Fever, trouble swallowing, excessive drooling, disorientation, convulsions, and even paralysis are physical indicators of rabies in dogs.
Your dog may exhibit extremely agitated behavior as the infection worsens, lights, motion, and noise appear to be distressing. They may wish to hide in a quiet, dark area or show violent behavior.
Foaming around the mouth is among the most well-known signs of canine rabies. Some canines may drool excessively or show extra saliva instead of "foaming."
This indicates that the infection has advanced. Seizures and progressive paralysis are frequent in the later stages of rabies. It is challenging for dogs to swallow during this period because they are unable to control their muscles, especially those in their head and neck.
Eventually, the ability to breathe is lost, which results in death.
Weeks may pass before your dog exhibits any symptoms of the infection in their body. The incubation period might be somewhat shorter or longer, although most cases in dogs manifest between 21 and 80 days following exposure.
It is essential to call a veterinarian before waiting to see any symptoms after your dog has been bitten.
How is it diagnosed and treated?
A blood test cannot reliably identify rabies. Testing is not possible until the dog has passed away since it involves a sample of brain tissue to be completely accurate.
When symptoms start, rabies in dogs cannot be treated. Sadly, your dog can be put to sleep if your veterinarian detects rabies since they could transmit the disease.
To reduce the likelihood that your dog will get the virus after being bitten by a wild animal, a booster dose of the rabies vaccine may be administered.
Preventive measures
Vaccinating your pet on time is the greatest approach to protect them from rabies. In fact, several countries require pets to have a rabies vaccination.
The vaccination benefits your dog in a variety of ways. In addition to protecting your pet from rabies, vaccinations also prevent them from harm if they accidentally bite somebody.
If your pet bites a person or another animal, the first thing that will be questioned of you is whether or not your pet has had all of his/her shots.
You can be certain that there is no risk of rabies spread by demonstrating that your pet has received the rabies vaccine. However, due to the potential risk, if your dog's immunizations are out-of-date, they might be put in isolation or possibly put down.
Animals who have injured people must be held for at least ten days in order to monitor the development of rabies.
Limiting interaction with wild animals can help you from contracting rabies.
Always be mindful of your surroundings and leash your dog when walking. Free-ranging animals are more prone to encounter wild animals and contract the disease.
Don't touch or disinfect your dog's wound if he was bitten, without gloves, since rabies can be transmitted this way.

Rabies
It is an incurable virus that attacks the brain and spinal cord. All mammals are susceptible to rabies. Even if it is preventable by vaccine and even treatable very early on, once the symptoms appear there is only an inevitable end.
How does it spread?
Since rabies is usually spread by a bite wound from an infected animal since it is produced in saliva. The virus invades the bloodstream when the skin is punctured by a bite. It can also spread through an open sore that is licked by an infected animal and exposed to its saliva.
Although it can spread from pet to pet, interaction with wild animals like bats, raccoons, and foxes is the main cause of rabies in dogs.
About 400 to 500 cases of rabies in household pets such cats, dogs, and ferrets are reported each year. Due to vaccination, rabies is entirely preventable in dogs in the U.s, hence it is not particularly prevalent.
Symptoms
Watch closely your dog's actions and call your veterinarian right away if you have any suspicions of rabies or if your dog has been injured by another animal and you feel worried about it.
Your dog might exhibit hostility while also quickly becoming aggressive and restless. Animals that are rabid may also exhibit unusually warm behavior (affectionate). Similar to this, your dog could appear relaxed and uninterested if they are typically joyful and excited. Fever, trouble swallowing, excessive drooling, disorientation, convulsions, and even paralysis are physical indicators of rabies in dogs.
Your dog may exhibit extremely agitated behavior as the infection worsens, lights, motion, and noise appear to be distressing. They may wish to hide in a quiet, dark area or show violent behavior.
Foaming around the mouth is among the most well-known signs of canine rabies. Some canines may drool excessively or show extra saliva instead of "foaming." This indicates that the infection has advanced. Seizures and progressive paralysis are frequent in the later stages of rabies. It is challenging for dogs to swallow during this period because they are unable to control their muscles, especially those in their head and neck. Eventually, the ability to breathe is lost, which results in death.
Weeks may pass before your dog exhibits any symptoms of the infection in their body. The incubation period might be somewhat shorter or longer, although most cases in dogs manifest between 21 and 80 days following exposure.
It is essential to call a veterinarian before waiting to see any symptoms after your dog has been bitten.
How is it diagnosed and treated?
A blood test cannot reliably identify rabies. Testing is not possible until the dog has passed away since it involves a sample of brain tissue to be completely accurate.
When symptoms start, rabies in dogs cannot be treated. Sadly, your dog can be put to sleep if your veterinarian detects rabies since they could transmit the disease.
To reduce the likelihood that your dog will get the virus after being bitten by a wild animal, a booster dose of the rabies vaccine may be administered.
Preventive measures
Vaccinating your pet on time is the greatest approach to protect them from rabies. In fact, several countries require pets to have a rabies vaccination.
The vaccination benefits your dog in a variety of ways. In addition to protecting your pet from rabies, vaccinations also prevent them from harm if they accidentally bite somebody. If your pet bites a person or another animal, the first thing that will be questioned of you is whether or not your pet has had all of his/her shots.
You can be certain that there is no risk of rabies spread by demonstrating that your pet has received the rabies vaccine. However, due to the potential risk, if your dog's immunizations are out-of-date, they might be put in isolation or possibly put down.
Animals who have injured people must be held for at least ten days in order to monitor the development of rabies.
Limiting interaction with wild animals can help you from contracting rabies. Always be mindful of your surroundings and leash your dog when walking. Free-ranging animals are more prone to encounter wild animals and contract the disease.
Don't touch or disinfect your dog's wound if he was bitten, without gloves, since rabies can be transmitted this way.


Lyme disease
Tick bites can lead to Lyme disease in dogs. The Lyme disease parasite is transmitted throughout the body after it enters the bloodstream and is most likely to settle in the joints or kidneys.
The deer tick is the most prevalent form of tick to carry Lyme disease (also known as the black-legged tick). In southern Sweden, it is extremely widespread.
People can also get affected, due to direct contact (being bitten) by the same tick that has bitten your dog.
How does it spread?
Ticks cannot infect people or other pets if they are already attached to someone, but they can detach and jump on the next host to feed on them and transmit the Lyme Disease bacteria into their host's bloodstream.
Symptoms
Within 3 to 30 days, some persons with Lyme disease experience the recognizable bull's-eye reaction at the location of the bite. If this happens, the condition can be quickly and accurately diagnosed.
However, compared to humans, animals have a harder time showing symptoms of Lyme disease. Dogs and cats do not develop the typical rash. In cats, Lyme illness is incredibly uncommon.
Many Lyme-infected dogs are brought to the vet because they appear to be in widespread pain and refused to eat. Dogs that are affected have been characterized as walking on eggshells.
These pets frequently have high fevers. Dogs may start limping as well.
This excruciating lameness frequently develops out of nowhere and may switch legs. If left unhealed, it can finally go away only to come back a few weeks or months later.
Before showing symptoms, some pets with the Lyme disease organism have been infected for over a year.
The illness may already be spreading throughout the body at this point. Vomiting, fatigue, anorexia (decreased appetite), and weight loss are non-specific symptoms suggesting Lyme disease may be harming the kidneys. The kidney form of the disease is rare, but it is often fatal when it occurs.
How is it diagnosed?
Lyme disease has various symptoms in dogs such as lameness, swollen joints, and fever. However, similar symptoms might also be brought on by other illnesses.
Several blood tests can be applied for confirmation. First, a particular test kit from your veterinarian can be used to conduct an antibody test in a clinic environment. This examination analyzes the antibodies produced as a result of exposure to the pathogen.
If the dog is infected but has not yet produced antibodies, or if it never produces enough antibodies to trigger a positive reaction, a test may result in a false negative. It is advised to get tested four weeks after being bitten by a tick.
Some dogs with long-lasting infections could no longer have enough antibodies to be identified by the test. A positive test is therefore significant, but a negative result is not.
To validate the antibody level, a QC6 test, and a follow-up examination can be performed.
With varying degrees of sensitivity, other tests such as the PCR (polymerase chain reaction), ELISA (enzyme-linked immunosorbent assay), joint fluid analysis, and culture can also be performed but are less frequent.
To evaluate kidney function and check for protein loss in the urine, general blood and urine tests are frequently performed.-link
How is it treated?
Since the Lyme spirochete is a bacterium, antibiotics can be used to treat it. Doxycycline is the preferred antibiotic, followed by amoxicillin and azithromycin.
Four weeks pass throughout treatment. Sometimes the original infection can come back, or the animal will get sick again after being bitten by another infected tick.
Preventive measures
Protecting your pet from being bitten by ticks is the key to prevention. In grassy, forested, and sandy environments, ticks are to be found.
They ascend small trees, especially cedar trees, leaves, grass blades, or other objects to reach an animal.
Here, they wait until an approaching animal is detected by their sensors before they crawl or descend. Keeping animals away from dense underbrush lowers their risk of being bitten by ticks.
When walking dogs close to woodland or tall grass regions, they should stay on the pathways.
Pets who reside in endemic regions or who travel to regions where Lyme disease is common should get vaccinated against it.
A number of products are also readily accessible that can aid in eliminating these ticks and reducing the risk of disease transmission.
While certain products can be purchased without a prescription, others can only be obtained from your veterinarian.
These external parasites can be easily controlled with efficient monthly preventatives, which are commonly administered to the epidermis at the bottom of the neck.
To maintain your pet parasite-free, your veterinarian will provide precise suggestions.
How do you remove a tick from a dog?
Once your pet has visited an area where ticks are present, check him/her right away. Approximately the size of a pinhead when young, the deer tick becomes slightly more noticeable as it ages and feeds.
A tick that is wandering on your pet has not been fed. The tick should be quickly removed and either crushed between two solid objects or placed in rubbing alcohol.
If you detect a tick on your pet, firmly grip it close to the dog's skin with your fingertips or fine tweezers and remove it straight out.
Twisting or shaking the tick could cause the mouthpieces to separate and stay in the skin. If you are unsure about the tick removal, it is best to go to a veterinarian to get help.
Make sure you use a tissue or a disposable glove to cover your fingers to prevent exposure.
Your dog may need further assistance being restrained.
Since the illness does not appear to be transferred until the tick has fed for around 12 hours, it is crucial to remove the tick as soon as possible.
Avoid getting the tick's fluids, including blood, on your skin if you decide to crush it.
A skin wound or cut can allow the bacterium that causes Lyme disease to enter your body.
There is a vaccine against the illness that is provided for dogs, and it is administered twice at distances of two to four weeks. After that, yearly immunization is required to preserve resistance.
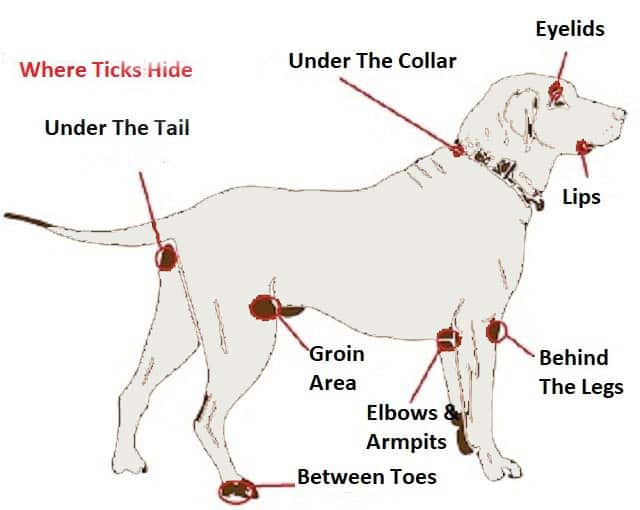

Lyme disease
Tick bites can lead to Lyme disease in dogs. The Lyme disease parasite is transmitted throughout the body after it enters the bloodstream and is most likely to settle in the joints or kidneys. The deer tick is the most prevalent form of tick to carry Lyme disease (also known as the black-legged tick). In southern Sweden, it is extremely widespread.
People can also get affected, due to direct contact (being bitten) by the same tick that has bitten your dog.
How does it spread?
Ticks cannot infect people or other pets if they are already attached to someone, but they can detach and jump on the next host to feed on them and transmit the Lyme Disease bacteria into their host's bloodstream.
Symptoms
Within 3 to 30 days, some persons with Lyme disease experience the recognizable bull's-eye reaction at the location of the bite. If this happens, the condition can be quickly and accurately diagnosed.
However, compared to humans, animals have a harder time showing symptoms of Lyme disease. Dogs and cats do not develop the typical rash. In cats, Lyme illness is incredibly uncommon.
Many Lyme-infected dogs are brought to the vet because they appear to be in widespread pain and refused to eat. Dogs that are affected have been characterized as walking on eggshells. These pets frequently have high fevers. Dogs may start limping as well. This excruciating lameness frequently develops out of nowhere and may switch legs. If left unhealed, it can finally go away only to come back a few weeks or months later.
Before showing symptoms, some pets with the Lyme disease organism have been infected for over a year. The illness may already be spreading throughout the body at this point. Vomiting, fatigue, anorexia (decreased appetite), and weight loss are non-specific symptoms suggesting Lyme disease may be harming the kidneys. The kidney form of the disease is rare, but it is often fatal when it occurs.
How is it diagnosed?
Lyme disease has various symptoms in dogs such as lameness, swollen joints, and fever. However, similar symptoms might also be brought on by other illnesses. Several blood tests can be applied for confirmation. First, a particular test kit from your veterinarian can be used to conduct an antibody test in a clinic environment. This examination analyzes the antibodies produced as a result of exposure to the pathogen. If the dog is infected but has not yet produced antibodies, or if it never produces enough antibodies to trigger a positive reaction, a test may result in a false negative. It is advised to get tested four weeks after being bitten by a tick.
Some dogs with long-lasting infections could no longer have enough antibodies to be identified by the test. A positive test is therefore significant, but a negative result is not. To validate the antibody level, a QC6 test, and a follow-up examination can be performed.
With varying degrees of sensitivity, other tests such as the PCR (polymerase chain reaction), ELISA (enzyme-linked immunosorbent assay), joint fluid analysis, and culture can also be performed but are less frequent. To evaluate kidney function and check for protein loss in the urine, general blood and urine tests are frequently performed.-link
How is it treated?
Since the Lyme spirochete is a bacterium, antibiotics can be used to treat it. Doxycycline is the preferred antibiotic, followed by amoxicillin and azithromycin. Four weeks pass throughout treatment. Sometimes the original infection can come back, or the animal will get sick again after being bitten by another infected tick.
Preventive measures
Protecting your pet from being bitten by ticks is the key to prevention. In grassy, forested, and sandy environments, ticks are to be found. They ascend small trees, especially cedar trees, leaves, grass blades, or other objects to reach an animal. Here, they wait until an approaching animal is detected by their sensors before they crawl or descend. Keeping animals away from dense underbrush lowers their risk of being bitten by ticks. When walking dogs close to woodland or tall grass regions, they should stay on the pathways. Pets who reside in endemic regions or who travel to regions where Lyme disease is common should get vaccinated against it.
A number of products are also readily accessible that can aid in eliminating these ticks and reducing the risk of disease transmission. While certain products can be purchased without a prescription, others can only be obtained from your veterinarian. These external parasites can be easily controlled with efficient monthly preventatives, which are commonly administered to the epidermis at the bottom of the neck. To maintain your pet parasite-free, your veterinarian will provide precise suggestions.
How do you remove a tick from a dog?
Once your pet has visited an area where ticks are present, check him/her right away. Approximately the size of a pinhead when young, the deer tick becomes slightly more noticeable as it ages and feeds. A tick that is wandering on your pet has not been fed. The tick should be quickly removed and either crushed between two solid objects or placed in rubbing alcohol. If you detect a tick on your pet, firmly grip it close to the dog's skin with your fingertips or fine tweezers and remove it straight out.
Twisting or shaking the tick could cause the mouthpieces to separate and stay in the skin. If you are unsure about the tick removal, it is best to go to a veterinarian to get help.
Make sure you use a tissue or a disposable glove to cover your fingers to prevent exposure.
Your dog may need further assistance being restrained. Since the illness does not appear to be transferred until the tick has fed for around 12 hours, it is crucial to remove the tick as soon as possible. Avoid getting the tick's fluids, including blood, on your skin if you decide to crush it.
A skin wound or cut can allow the bacterium that causes Lyme disease to enter your body.
There is a vaccine against the illness that is provided for dogs, and it is administered twice at distances of two to four weeks. After that, yearly immunization is required to preserve resistance.
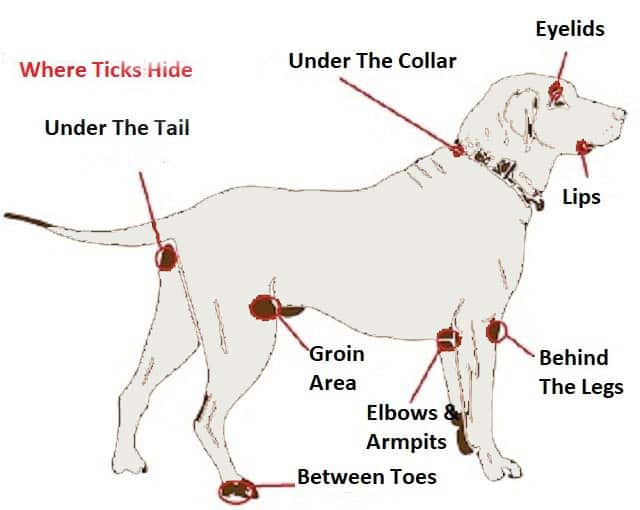
BORDETELLA BRONCHISEPTICA (KENNEL COUGH)
Kennel cough is a common respiratory disease in dogs. It can be caused by different bacterias and viruses at the same time (for example Bordetella bronchiseptica-being the most common cause, parainfluenza virus, adenovirus type 2, or canine coronavirus).
These irritate and inflame the dog's upper airway by attacking the membrane of the dog's respiratory system. In generally healthy canines, this condition is not harmful.
However, it can cause more severe secondary infections in young puppies, elderly dogs, or canines who already have compromised immune systems.
Kennel cough is a word used to describe how contagious this illness is.
In environments where animals are in close proximity to one another, such as kennels, dog parks, and multi-dog residences, it spreads rapidly.
When dogs come into proximity with fluids from an ill dog, kennel cough can spread.
Direct touch with the sick dog or objects that have picked up contaminated droplets can cause this. These might be blankets, bowls, cages, or toys for dogs.
How does it spread?
Dogs can easily spread kennel cough through casual contact, such as smelling each other when out for a walk, playing, or sharing water bowls.
The probability that your dog will have kennel cough is increased by a few things, such as stress, chilly weather, contact with dust or smoke, and overcrowded surroundings.
Symptoms
A persistent, non-productive dry cough is the main sign of kennel cough.
Typically, it sounds like a goose honking or as if your dog's throat is blocked with something.
Other symptoms include a runny nose, sneezing, general fatigue, decreased appetite, and a moderate temperature.
Keep your dog away from other dogs if they show signs of kennel cough. For advice, speak with your vet immediately away.
Your veterinarian might advise keeping your dog away from other dogs because the disease is contagious.
This enables you to monitor your dog's symptoms while allowing him/her to relax for a few days.
On the other hand, your veterinarian could advise bringing your dog in for a checkup if the symptoms are more serious.
How is it diagnosed?
A method of elimination is used to identify kennel cough. Your veterinarian will initially check your pet for signs of a collapsed trachea, heartworm disease, pneumonia, asthma, cancer, heart disease, and other disorders because kennel cough symptoms are similar to those of many more serious illnesses.
Coughing may also indicate the presence of the canine distemper or influenza viruses.
Your veterinarian will decide if kennel cough is the primary culprit of your dog's symptoms based on the examination results and medical history.
How is it treated?
Healthy adult dogs can be treated for kennel cough. Your veterinarian may decide that rest is the best medicine while the disease runs its course and that no drugs are necessary (much like the human cold).
Veterinarians may recommend antibiotics to help avoid subsequent infections or cough suppressants to assist your dog's chronic coughing if they notice more severe symptoms.
When taking your pet for walks while they are mending, it is best to refrain from utilizing neck collars and instead utilize a body harness.
Additionally, since a humidifier can assist your dog's problems, you may wish to use one in the areas where he spends time.
The disease can last up to two weeks, although there are some rare cases when kennel cough develops into pneumonia.
Preventive measures
Immunization against bordetella is also strongly advised for dogs who are boarded, groomed, or have contact with other dogs in settings like dog parks.
Even if the dog has gone through a natural infection, their resistance is neither strong nor long-lasting. We cannot hope for substantially better results from immunizations.
To guarantee optimum defense against this unpleasant virus, several kennel facilities demand a booster immunization just before boarding, and other veterinarians advise a booster vaccination every 6 months.
Immunization against bordetella can be administered orally, intra-nasal, or by injection.
The term "intra-nasal" describes the liquid vaccine given as nose drops. The oral form can be administered in the cheek pouch.
This offers quicker infection protection than the injectable vaccination by allowing local immunity to build on the mucosal membranes of the nose, throat, and trachea where the pathogens initially strike.

BORDETELLA BRONCHISEPTICA (KENNEL COUGH)
Kennel cough is a common respiratory disease in dogs. It can be caused by different bacterias and viruses at the same time (for example Bordetella bronchiseptica-being the most common cause, parainfluenza virus, adenovirus type 2, or canine coronavirus).
These irritate and inflame the dog's upper airway by attacking the membrane of the dog's respiratory system. In generally healthy canines, this condition is not harmful. However, it can cause more severe secondary infections in young puppies, elderly dogs, or canines who already have compromised immune systems.
Kennel cough is a word used to describe how contagious this illness is. In environments where animals are in close proximity to one another, such as kennels, dog parks, and multi-dog residences, it spreads rapidly. When dogs come into proximity with fluids from an ill dog, kennel cough can spread. Direct touch with the sick dog or objects that have picked up contaminated droplets can cause this. These might be blankets, bowls, cages, or toys for dogs.
How does it spread?
Dogs can easily spread kennel cough through casual contact, such as smelling each other when out for a walk, playing, or sharing water bowls. The probability that your dog will have kennel cough is increased by a few things, such as stress, chilly weather, contact with dust or smoke, and overcrowded surroundings.
Symptoms
A persistent, non-productive dry cough is the main sign of kennel cough. Typically, it sounds like a goose honking or as if your dog's throat is blocked with something. Other symptoms include a runny nose, sneezing, general fatigue, decreased appetite, and a moderate temperature.
Keep your dog away from other dogs if they show signs of kennel cough. For advice, speak with your vet immediately away.
Your veterinarian might advise keeping your dog away from other dogs because the disease is contagious. This enables you to monitor your dog's symptoms while allowing him/her to relax for a few days.
On the other hand, your veterinarian could advise bringing your dog in for a checkup if the symptoms are more serious.
How is it diagnosed?
A method of elimination is used to identify kennel cough. Your veterinarian will initially check your pet for signs of a collapsed trachea, heartworm disease, pneumonia, asthma, cancer, heart disease, and other disorders because kennel cough symptoms are similar to those of many more serious illnesses. Coughing may also indicate the presence of the canine distemper or influenza viruses.
Your veterinarian will decide if kennel cough is the primary culprit of your dog's symptoms based on the examination results and medical history.
How is it treated?
Healthy adult dogs can be treated for kennel cough. Your veterinarian may decide that rest is the best medicine while the disease runs its course and that no drugs are necessary (much like the human cold).
Veterinarians may recommend antibiotics to help avoid subsequent infections or cough suppressants to assist your dog's chronic coughing if they notice more severe symptoms.
When taking your pet for walks while they are mending, it is best to refrain from utilizing neck collars and instead utilize a body harness. Additionally, since a humidifier can assist your dog's problems, you may wish to use one in the areas where he spends time.
The disease can last up to two weeks, although there are some rare cases when kennel cough develops into pneumonia.
Preventive measures
Immunization against bordetella is also strongly advised for dogs who are boarded, groomed, or have contact with other dogs in settings like dog parks.
Even if the dog has gone through a natural infection, their resistance is neither strong nor long-lasting. We cannot hope for substantially better results from immunizations. To guarantee optimum defense against this unpleasant virus, several kennel facilities demand a booster immunization just before boarding, and other veterinarians advise a booster vaccination every 6 months.
Immunization against bordetella can be administered orally, intra-nasal, or by injection. The term "intra-nasal" describes the liquid vaccine given as nose drops. The oral form can be administered in the cheek pouch. This offers quicker infection protection than the injectable vaccination by allowing local immunity to build on the mucosal membranes of the nose, throat, and trachea where the pathogens initially strike.

Parainfluenza Virus
One of the most frequent contributing causes of Kennel cough (infectious tracheobronchitis), an acute or chronic inflammation of the respiratory airways, is the highly contagious canine parainfluenza virus.
How does it spread?
CPIV is spread through contact with infected food bowls, water bowls, and bedding as well as airborne particles from coughing and sneezing. Even after recovery, an infected dog might spread the infection for up to two weeks.
Dogs who are positioned close to an infected dog run the danger of contracting canine parainfluenza. Boarding kennels, breeding kennels, rehoming shelters, pet daycare facilities, dog parks, and groomers are a few locations where this could happen.
Canine adenovirus-2 (CAV-2) and Bordetella bronchiseptica, as well as parainfluenza, may cause kennel cough in dogs.
Symptoms
Although the symptoms of CPIV match those of canine influenza, this virus requires entirely different medical care and immunizations. Depending on the dog's age and any underlying illnesses or compromised immunity, canine parainfluenza symptoms can change. Any or all of the following symptoms could be present:
Continuous cough
Fever
Nasal discharge
Sneezing
Eye irritation
Lethargy
Reduced appetite
How is it diagnosed?
Get your dog checked out by a veterinarian as soon as you can if he is exhibiting symptoms of CPIV infection. Your pet will undergo a comprehensive examination from your veterinarian, who will also ask you for a full medical history, a list of your pet's symptoms, and the date those symptoms first arose. You must also describe any close interactions he has had in the past month with other dogs. In order to test for the virus and rule out any other infections, a blood sample and/or a secretion sample from the eye or nose will be collected. An x-ray of the chest may be recommended by your veterinarian if there are worries that your pet has pneumonia. Effective therapy for your dog depends on a quick diagnosis.
How is it treated?
Despite the fact that some dogs may recuperate from the infection without treatment, it is usually advisable to heal any bacterial infections with antibiotics and suppress viral infections with antiviral drugs. Cough suppressants and painkillers are likely to be prescribed if your dog has a very severe, dry cough since prolonged coughing can damage the lung tissue and lead to long-term issues.
The speed of treatment and diagnosis as well as your dog's condition previous to the illness, will all be crucial factors in his recovery. Maintaining your pet's isolation will shield him from problems and any subsequent illnesses in addition to preventing the virus from spreading further.
Within two weeks, the infection should be completely gone.
Preventive measures
There is an available vaccine that is effective to prevent these disease, although it is not part of a regular immunization process. If you have any concerns about your dog interacting with others, you can ask your veterinarian about the importance of this type of vaccine.

Canine Influenza Virus
Canine influenza virus, often known as dog flu, is a contagious respiratory illness brought on by an influenza A virus that is related to the strains of the virus that cause human influenza. There are two recognized dog flu strains in the country:
H3N8
H3N2
Horses are where the H3N8 strain truly came from. By 2004, when the first epidemics hit racing Greyhounds at a racetrack in Florida, the virus crossed over from infecting horses to infecting dogs, evolving into a canine influenza virus.
H3N2, in contrast , is thought to have its origins in Asia, where it spread from birds to dogs. The Midwest saw canine influenza outbreaks in 2015 and 2016, and the H3N2 virus is still circulating across the country.
How does it spread?
Dog flu is an airborne illness, just like influenza in humans. Coughing, barking, and sneezing are examples of respiratory secretions escaping into the environment where they are then breathed by a new canine host.
The canine flu can also spread through interaction with people who have had close touch with an infected dog as well as through contaminated water bowls, collars, and kennel surfaces.
Infections like canine influenza thrive in crowded settings like kennels, grooming salons, daycare facilities, and dog parks.
Due to the dogs' close contact, one dog's barking, coughing, or sneezing can readily spread to dogs nearby. Given that canines are most infectious during the incubation time before they develop symptoms, this is made even more severe.
Although almost all infected dogs will get the disease, not all infected dogs will display viral symptoms. Twenty to twenty-five percent of infected dogs do not exhibit any symptoms, yet they can still spread the disease. Your dogs may still be infected even if one of them develops the virus while the other seems unharmed.
Symptoms
Coughing (both moist and dry)
Sneezing
Nasal discharge
Purulent nasal discharge
Eye discharge
Fever\Lethargy
Having trouble breathing
The symptoms of dog flu are similar to those of kennel cough, which is another ailment you should discuss with your veterinarian as soon as you see symptoms.
Severe cases are rare-in these cases dogs develop pneumonia, difficulty breathing, and high fever, although the mortality rate is low-less than 10%.
How is it diagnosed?
Canine influenza is difficult to distinguish from other respiratory illnesses based only on clinical indications. A nasal swab can be given to a veterinary diagnostic lab for a polymerase chain reaction (PCR) test if a veterinarian meets a dog during the first few days of the development of clinical indications. The dog most likely has CIV if the PCR test is positive. PCR results are less likely to be accurate after 4 days of illness (there may be false-negative results).
Blood tests for CIV antibodies ought to be done at this point. This sort of testing, known as serology, compares antibody levels obtained two to three weeks apart. If antibody levels increase dramatically during this time, CIV infection is active. The veterinarian may also need to run some blood work and radiographs to understand the gravity of the disease.
How is it treated?
Similar to almost other viral infections, the majority of the treatment is supportive. When your pet is sick, it's crucial that they are kept in a warm, dry area separate from other dogs, provided a high-quality meal, and kept hydrated.
For dogs to generate a sufficient immune response and to recover more quickly, proper nutrition and care are essential.
When a dog has a moderate case of canine influenza, bacterial upper respiratory infections frequently follow. These dogs benefit from broad-spectrum antibiotic medication and frequently have a thick, green mucus discharge from their noses.
When a dog develops pneumonia, hospitalization, intravenous fluids, and medicines, as well as strong broad-spectrum antibiotics, may be necessary. The majority of canines recover totally from canine influenza in 2 to 3 weeks. Further isolation for 4 weeks is needed.
Preventive measures
If you think you had any contact with an infected dog it is essential to clean your hands, arms and clothes before coming into contact with your dog.
Vaccinations against the two influenza strands (H3N8 AND H3N2) are available and based on your and your dog's lifestyle (if you meet often a lot of dogs, travel, go to grooming salons or visit crowded places), your veterinarian will recommend a suitable vaccine.

Parainfluenza Virus
One of the most frequent contributing causes of Kennel cough (infectious tracheobronchitis), an acute or chronic inflammation of the respiratory airways, is the highly contagious canine parainfluenza virus.
How does it spread?
CPIV is spread through contact with infected food bowls, water bowls, and bedding as well as airborne particles from coughing and sneezing. Even after recovery, an infected dog might spread the infection for up to two weeks.
Dogs who are positioned close to an infected dog run the danger of contracting canine parainfluenza. Boarding kennels, breeding kennels, rehoming shelters, pet daycare facilities, dog parks, and groomers are a few locations where this could happen.
Canine adenovirus-2 (CAV-2) and Bordetella bronchiseptica, as well as parainfluenza, may cause kennel cough in dogs.
Symptoms
Although the symptoms of CPIV match those of canine influenza, this virus requires entirely different medical care and immunizations. Depending on the dog's age and any underlying illnesses or compromised immunity, canine parainfluenza symptoms can change. Any or all of the following symptoms could be present:
Continuous cough
Fever
Nasal discharge
Sneezing
Eye irritation
Lethargy
Reduced appetite
How is it diagnosed?
Get your dog checked out by a veterinarian as soon as you can if he is exhibiting symptoms of CPIV infection.
Your pet will undergo a comprehensive examination from your veterinarian, who will also ask you for a full medical history, a list of your pet's symptoms, and the date those symptoms first arose.
You must also describe any close interactions he has had in the past month with other dogs.
In order to test for the virus and rule out any other infections, a blood sample and/or a secretion sample from the eye or nose will be collected.
An x-ray of the chest may be recommended by your veterinarian if there are worries that your pet has pneumonia. Effective therapy for your dog depends on a quick diagnosis.
How is it treated?
Despite the fact that some dogs may recuperate from the infection without treatment, it is usually advisable to heal any bacterial infections with antibiotics and suppress viral infections with antiviral drugs.
Cough suppressants and painkillers are likely to be prescribed if your dog has a very severe, dry cough since prolonged coughing can damage the lung tissue and lead to long-term issues.
The speed of treatment and diagnosis as well as your dog's condition previous to the illness, will all be crucial factors in his recovery.
Maintaining your pet's isolation will shield him from problems and any subsequent illnesses in addition to preventing the virus from spreading further.
Within two weeks, the infection should be completely gone.
Preventive measures
There is an available vaccine that is effective to prevent these disease, although it is not part of a regular immunization process.
If you have any concerns about your dog interacting with others, you can ask your veterinarian about the importance of this type of vaccine.

Canine Influenza Virus
Canine influenza virus, often known as dog flu, is a contagious respiratory illness brought on by an influenza A virus that is related to the strains of the virus that cause human influenza. There are two recognized dog flu strains in the country:
H3N8
H3N2
Horses are where the H3N8 strain truly came from. By 2004, when the first epidemics hit racing Greyhounds at a racetrack in Florida, the virus crossed over from infecting horses to infecting dogs, evolving into a canine influenza virus.
H3N2, in contrast , is thought to have its origins in Asia, where it spread from birds to dogs. The Midwest saw canine influenza outbreaks in 2015 and 2016, and the H3N2 virus is still circulating across the country.
How does it spread?
Dog flu is an airborne illness, just like influenza in humans. Coughing, barking, and sneezing are examples of respiratory secretions escaping into the environment where they are then breathed by a new canine host.
The canine flu can also spread through interaction with people who have had close touch with an infected dog as well as through contaminated water bowls, collars, and kennel surfaces.
Infections like canine influenza thrive in crowded settings like kennels, grooming salons, daycare facilities, and dog parks.
Due to the dogs' close contact, one dog's barking, coughing, or sneezing can readily spread to dogs nearby. Given that canines are most infectious during the incubation time before they develop symptoms, this is made even more severe.
Although almost all infected dogs will get the disease, not all infected dogs will display viral symptoms.
Twenty to twenty-five percent of infected dogs do not exhibit any symptoms, yet they can still spread the disease. Your dogs may still be infected even if one of them develops the virus while the other seems unharmed.
Symptoms
Coughing (both moist and dry)
Sneezing
Nasal discharge
Purulent nasal discharge
Eye discharge
Fever\Lethargy
Having trouble breathing
The symptoms of dog flu are similar to those of kennel cough, which is another ailment you should discuss with your veterinarian as soon as you see symptoms.
Severe cases are rare-in these cases dogs develop pneumonia, difficulty breathing, and high fever, although the mortality rate is low-less than 10%.
How is it diagnosed?
Canine influenza is difficult to distinguish from other respiratory illnesses based only on clinical indications.
A nasal swab can be given to a veterinary diagnostic lab for a polymerase chain reaction (PCR) test if a veterinarian meets a dog during the first few days of the development of clinical indications. The dog most likely has CIV if the PCR test is positive.
PCR results are less likely to be accurate after 4 days of illness (there may be false-negative results).
Blood tests for CIV antibodies ought to be done at this point. This sort of testing, known as serology, compares antibody levels obtained two to three weeks apart.
If antibody levels increase dramatically during this time, CIV infection is active.
The veterinarian may also need to run some blood work and radiographs to understand the gravity of the disease.
How is it treated?
Similar to almost other viral infections, the majority of the treatment is supportive.
When your pet is sick, it's crucial that they are kept in a warm, dry area separate from other dogs, provided a high-quality meal, and kept hydrated.
For dogs to generate a sufficient immune response and to recover more quickly, proper nutrition and care are essential.
When a dog has a moderate case of canine influenza, bacterial upper respiratory infections frequently follow.
These dogs benefit from broad-spectrum antibiotic medication and frequently have a thick, green mucus discharge from their noses.
When a dog develops pneumonia, hospitalization, intravenous fluids, and medicines, as well as strong broad-spectrum antibiotics, may be necessary.
The majority of canines recover totally from canine influenza in 2 to 3 weeks. Further isolation for 4 weeks is needed.
Preventive measures
If you think you had any contact with an infected dog it is essential to clean your hands, arms and clothes before coming into contact with your dog.
Vaccinations against the two influenza strands (H3N8 AND H3N2) are available and based on your and your dog's lifestyle (if you meet often a lot of dogs, travel, go to grooming salons or visit crowded places), your veterinarian will recommend a suitable vaccine.

Until one has loved an animal, a part of one’s soul remains unawakened.
Anatole France
Until one has loved an animal, a part of one’s soul remains unawakened.
Anatole France
Reference
https://www.aaha.org/your-pet/pet-owner-education/ask-aaha/Pet-Vaccination/
https://de.luko.eu/en/advice/guide/puppy-vaccination-plan/
https://www.aaha.org/your-pet/pet-owner-education/ask-aaha/Pet-Vaccination/
https://www.avma.org/resources/pet-owners/petcare/canine-distemper
https://en.wikipedia.org/wiki/Canine_distemper
https://www.avma.org/resources-tools/pet-owners/petcare/canine-parvovirus
https://en.wikipedia.org/wiki/Canine_parvovirus
https://www.avma.org/resources/pet-owners/petcare/leptospirosis
https://pets.webmd.com/dogs/rabies-dogs
https://vcahospitals.com/know-your-pet/lyme-disease-in-dogs
https://www.americanvetonline.com/site/blog/2021/12/15/symptoms-kennel-cough-dogs
https://vcahospitals.com/know-your-pet/kennel-cough-or-tracheobronchitis-in-dogs
https://homehealth-uk.com/animalhealth/canine-parainfluenza-virus-cpiv/
https://vcahospitals.com/know-your-pet/canine-influenza-the-dog-flu
https://www.akc.org/expert-advice/health/the-dog-flu-symptoms-you-need-to-know/